Why am I Writing About the Rare Disease, Esophageal Diverticulum?
The short answer is because I was recently diagnosed with it, although symptoms have been accumulating for some time now. I had simply assumed that all the regurgitation and vomiting, even in the middle of the night, were due to acid reflux.
If not for an admission to the A&E/ER for something completely unrelated, the doctors would never have found it. The esophageal diverticulum was an incidental finding after I did a CT scan. According to Constantin et al. (2023), “somewhere between 0.06 – 4% [of epiphrenic esophageal diverticulum] are discovered incidentally, radiologically”.
Anyway, I have decided to split this into a two part series. I will publish more about my personal experiences with epiphrenic esophageal diverticulum soon. This post will focus entirely on research I’ve done thus far, as a patient.
*Disclaimer: This article is meant for educational purposes, and is based on my personal experiences as a patient. Whilst I have done my utmost to be meticulous in research, I am not a doctor, and nothing in this article should be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. This post may also contain affiliate links. It will cost you nothing to click on them. I will get a small referral fee from purchases you make, which helps with the maintenance of this blog. Read our Privacy Policy page for more information. Thank you!
Pin to Your Rare Disease & Chronic Illness Boards:

A Brief Look at the Esophagus / Oesophagus
In order to understand what certain terms mean and the implications of the different types of esophageal diverticulum, we first need to understand a bit about how the esophagus works. The esophagus is the “hollow, muscular tube that carries food and liquid from your throat to your stomach”, and is part of your digestive system (Cleveland Clinic, 2021b, August 4). It is approximately 9 to 10 inches long (23 to 25 cm).
The esophagus itself is made up of four layers – the mucosa, submucosa, muscularis and adventitia (Yam et al., 2023, April 24), and can be divided into three anatomical segments – cervical, thoracic and abdominal (Chaudhry and Bordoni, 2023, July 24).
Peristalsis
The main function of the esophagus is to transport food from the mouth to stomach, and it does that through a series of muscular contractions known as peristalsis, which is an automatic wave-like movement that happens within the digestive tract (Chaudhry and Bordoni, 2023, July 24; Cleveland Clinic, 2022, April 28).
According to Nehra et al. (2022), “the proximal one-third of the esophagus is composed of striated muscle, the distal one-third is composed of smooth muscle, and the middle one-third contains a mixture of striated and smooth muscle”.
Peristalsis in the different muscle types is controlled by different types of neuronal activity. The lower esophageal sphincter is also made up of smooth muscle segments. This allows for the smooth passing of food into the stomach, and also prevents gastroesophageal reflux (Nehra et al., 2022).
Some other keywords in relation to the esophagus are:
- Esophageal lumen – the inside of the esophagus
- Esophageal sphincter – a ring-shaped muscle that contracts and expands</li
- Mediastinum – The centre area of the chest between the lungs, where the esophagus, heart, thymus, trachea and other structures can be found (Cleveland Clinic, 2022b, August 29)
What is Esophageal Diverticulum?
Esophageal diverticulum is a rare disease with a prevalence of less than 1% globally (Yam et al., 2023, April 24). Patients with esophageal diverticulum have an outpouching within the esophagus, and the disorder is categorised based on anatomical location and type. ‘Diverticula’ is the plural term, where there are more than one diverticulum.
Esophageal Diverticulum Based on Anatomical Location
There are primarily three types of esophageal diverticula – Zenker’s, mid-esophageal and epiphrenic, running from top to bottom of the esophagus (Constantin et al., 2023).
Within the pharyngoesophageal space, they can be further categorised as – Zenker’s, Killian-Jamieson and Laimer’s, once again based on where they occur (Watanabe et al., 2023). Here is a great illustration that shows the differences between these three types of diverticulum, from a left lateral and posterior view (Zakaria and Barawi, 2020).
Then there is also a diffuse type, known as “diffuse intramural pseudodiverticulosis” (DEIPD) (Constantin et al., 2023), which is a “chronic, fibrosing inflammatory disease” (Hentschel, 2022). Iatrogenic diverticulum has also been added as a category recently. As its name suggests, it happens post treatment – peroral endoscopic myotomy (POEM)-type endoscopic therapy, in this instance. Such treatments are often used for late complications of achalasia (a swallowing disorder) (Constantin et al., 2023).
Whilst esophageal diverticulum is a rare disease, the most common tends to be Zenker’s diverticulum – the one that occurs at the top of the esophagus. Esophageal diverticula are also more commonly found in the elderly, and in men as opposed to women (Yam et al., 2023, April 24), so I guess that makes me one lucky dark unicorn again.
Esophageal Diverticulum by Type
There are two ways that an esophageal diverticulum forms – pulsion or traction, with the former being more common. ‘Pulsion’ simply means pushing, whilst ‘traction’ means pulling. Therefore, pulsion diverticula push against the esophageal wall, whereas traction diverticula are ‘sucked in’, which lead to the formation of indentations in the esophageal wall (Cleveland Clinic, 2023, September 29).
According to Sato et al. (2019), pulsion esophageal diverticula form due to “inadequate relaxation of either the upper esophageal sphincter (UES) or the lower esophageal sphincter (LES), causing an increase of intraluminal pressure resulting in a herniation of the esophageal wall in an area of low parietal resistance”. Traction esophageal diverticula on the other hand, involves “adhesion and traction on the esophageal wall in the presence of a mediastinal inflammatory focus, resulting in the formation of a diverticular pouch”.
To simplify that explanation, a pulsion esophageal diverticulum is due to pressure within the esophagus. This leads to an abnormal bulge in the weaker areas of the esophageal wall. Traction esophageal diverticulum on the other hand, is caused by inflammation within the mediastinum. This pulling effect leads to the formation of pouches within the esophagus.
True Versus False Diverticula
Esophageal diverticulum can be further classified as either ‘true’ or ‘false’. According to Yam et al. (2023, April 24), true diverticula involve all four layers of the esophageal wall, whereas only the mucosa and submucosa layers are involved in false diverticula.
True diverticula are caused by traction (pulling), whilst false diverticula by pulsion (pushing). In general, Zenker’s and epiphrenic diverticula are false diverticula, whilst mid-esophageal diverticula are true diverticula.
Some Charts for Easier Digestion (Pun Not Quite Intended)
You can view the correlation between esophageal typography, anatomo-clinical criteria and etiopathogeny in Table 2 here (Constantin et al., 2023).
Figure 1 in this paper by Sudarshan and Murthy (2021) also provides an excellent summary of the three main types of esophageal diverticula. It includes their varying pathophysiology, presentations, work-up and management for easy comparison.
Finally, you can view some images of how various esophageal diverticula look like on Radiopaedia (Rezaee, 2024, December 17).
Pin to Your Rare Disease & Medical Infographic Boards:
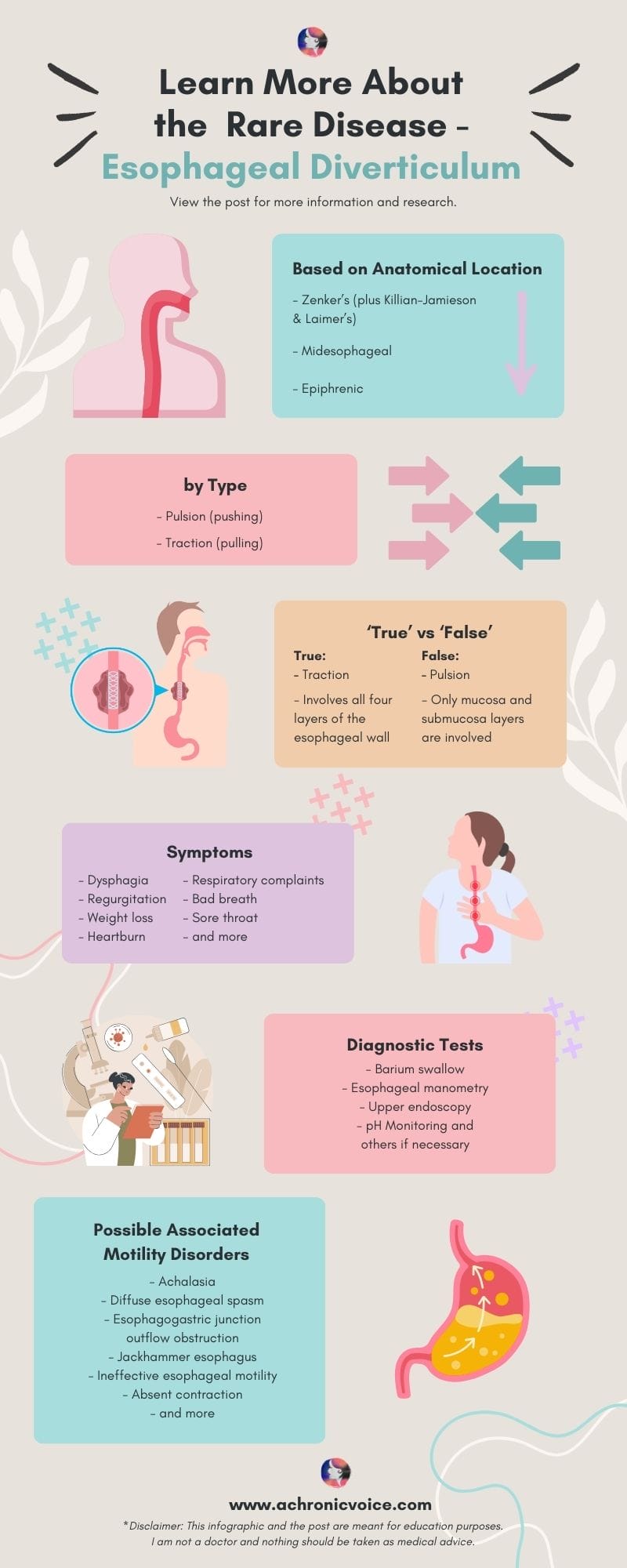
Esophageal Diverticulum Symptoms – From Mild to Severe
According to Sato et al. (2023), the main symptoms of esophageal diverticulum are “dysphagia, regurgitation, weight loss, heartburn, respiratory complaints, and retrosternal pain when swallowing food”.
The ‘milder’ symptoms of esophageal diverticulum include an irritating sensation in the throat as if something is stuck there, a sore throat and halitosis (bad breath). As the diverticulum increases in size over time, it can lead to other complications as food gets stuck in the pouches. For instance, patients can get “esophagitis, bleeding from ulceration, impaction, and stasis with regurgitation” (Sato et al., 2023).
Aspiration pneumonia can also happen especially when a person is asleep, where regurgitated food gets inhaled into the lungs and becomes infected. Apart from gastric content, the aspirated fluid can also consist of oropharyngeal secretions and particulate matter (Sanivarapu et al., 2024, March 20).
Aspiration pneumonia is also one of my biggest fears, as regurgitation at night is one of my main symptoms. According to Thomas et al. (2001), other serious manifestations of esophageal diverticulum include: “acute dyspnoea and stridor from pulmonary displacement, cardiac tachydysrhythmias from atrial compression and diverticular rupture, and, rarely, tension pneumothorax”.
In sum, esophageal diverticulum can potentially affect your heart, lungs, and their surrounding structures, due to pressure and/or rupture. It can also give rise to heart rhythm issues.
Whilst the formation of ulcers rarely leads to perforation or bleeding, such events can be life-threatening if they do happen. In addition, atypical symptoms of esophageal diverticulum may remain unknown until surgery is being done (Thomas et al., 2001).
Diagnosing Esophageal Diverticulum
After that incidental finding of the esophageal diverticula from the CT scan, I had to go for a barium swallow test. The surgeon has also mentioned that I will need to do a manometry and endoscopy as pre-operative procedures.
This is in line with what I have read up thus far within the medical literature. According to Herbella and Patti (2012), the preoperative workup for esophageal diverticulum treatment includes: a barium swallow test, endoscopy, manometry, and pH monitoring if deemed necessary (also see: Thomas et al., 2001).
Let’s take a look at these tests used to diagnose esophageal diverticulum and motility disorders, to better understand why they’re important.
Barium Swallow Test
In order to clearly see and define the esophageal diverticulum, a barium swallow test (esophagram) (MedlinePlus, 2024a, August 27) is usually carried out first. The patient will be made to drink a chalky liquid at intervals. This helps with the visualisation of the diverticulum by ‘highlighting’ it under fluoroscopy, which is a type of x-ray that shows the movement of organs in real-time (MedlinePlus, 2024b, August 27). From the test, your medical team will then be able to determine the size and location of the diverticulum, and also if they are on the right or left side of the esophagus (Sudarshan et al., 2021).
The information from the barium swallow test is important for determining the course of treatment, and type of surgical method to use. In general, surgery is avoided for asymptomatic patients due to the risks, although some surgeons think that it is still essential, as up to 45% of patients demonstrated aspiration (Sudarshan et al., 2021). Some also think surgery is necessary, due to the “risk of cancerization of the diverticulum mucosa or spontaneous rupture” (Sato et al., 2023).
In addition, a timed barium swallow test is able to detect certain motility disorders such as achalasia, as well as “associated conditions such as dysmotility, hiatal hernia, distal esophageal rings, and reflux” (Sudarshan and Murthy, 2021).
Esophageal Manometry
According to Gyawali et al. (2020), “esophageal manometry is generally considered the gold standard for the diagnosis of motility disorders”. It is important to get this diagnostic test done especially for epiphrenic esophageal diverticula, as these are often due to an esophageal motility disorder, such as achalasia or diffuse esophageal spasm (Alicuben et al., 2023).
The word “manometry” simply means a measurement of pressure. A tube will be placed down your nasal cavity and into your esophagus. Thereafter, you will be made to swallow water and/or other liquids of different consistencies, in various bodily positions (Cleveland Clinic, 2023, October 5).
A high-resolution manometry is usually recommended, based on the latest research (Sato et al., 2019). The difference between a regular and high-resolution manometry is that the latter uses more catheters (36 as opposed to 5), thus producing more accurate results (Yadlapati, 2017).
Upper Endoscopy (Esophagogastroduodenoscopy)
A preoperative upper endoscopy is essential for several reasons. First, to rule out other possible diseases (such as Barrett’s esophagus) or malignancies (cancers), and also to clear any debris stuck in the diverticula before surgery is done (Alicuben et al., 2023; Herbella and Patti, 2012).
The Importance of Differential Diagnosis and Detection of Motility Disorders
There are a number of other disorders that can mimic an esophageal diverticulum, and vice versa. A differential diagnosis is essential to rule out such cases. This is simply a process that takes into account all possible diagnoses based on your individual symptoms, medical history, lifestyle and more (MedlinePlus, 2023, February 27). Additional tests may be done if deemed necessary. This helps your medical team to conclude with a more definitive diagnosis, and therefore, the treatment course to take.
For epiphrenic esophageal diverticulum, the differential diagnosis includes: “hiatal hernia, esophageal webs and strictures, esophageal duplication cyst, and esophageal carcinoma”. Other differential diagnosis of underlying causes should also be ruled out as well, such as: “achalasia, distal esophageal spasm, ineffective esophageal motility, esophagogastric junction outflow obstruction, end-stage gastroesophageal (GE) reflux disease with a “burnt out” esophagus, peptic stricture, or failed previous fundoplication” (Alicuben et al., 2023).
Whilst rare, it is also important to screen for malignancies (cancers). The incidence of malignancies from esophageal diverticula is 0.3% to 7% for pharyngoesophageal (which includes Zenker’s), 1.8% for midesophageal, and 0.6% for epiphrenic (Herbella and Patti, 2012).
The Link Between Motility Disorders and Esophageal Diverticulum
As mentioned, motility disorders are often the underlying cause of esophageal diverticulum – particularly so in epiphrenic esophageal diverticulum. In fact, according to Thomas et al. (2001), one should still “remain suspicious” even if a motility disorder is not detected during medical investigations, as apart from achalasia, most of such disorders “occur intermittently and may not be evident during oesophagoscopy, contrast radiology or standard manometry”.
Studies have also shown that “more than 75% of epiphrenic diverticula occur concomitantly with esophageal motility disorders” (Sato et al., 2019). In one small study by Nehra et al. (2002), all their patients with epiphrenic esophageal diverticulum were found to have a motility disorder, using 24-hour ambulatory motility testing.
Achalasia – The Most Common Motility Disorder Found in Esophageal Diverticulum
Achalasia has been mentioned numerous times in this post. Achalasia is a rare swallowing disorder that stems from damaged nerves in the esophagus, specifically in the lower esophageal sphincter. As a result, food and liquid are unable to move down to the stomach. How achalasia develops is still unknown, but has been purported to be autoimmune in nature (Cleveland Clinic, 2021a, April 6).
There are also different types of achalasia based on manometric patterns, namely: type 1 (classic), type 2, and type 3 (spastic). Type 1 achalasia has “minimal contractility in the esophageal body”, Type 2 has “intermittent periods of panesophageal pressurization”, and Type 3 has “premature or spastic distal esophageal contractions”. They also vary in immunohistochemical markers and histology (Patel et al., 2017).
Achalasia is also the most common motility disorder found in patients with esophageal diverticulum (Herbella and Patti, 2012). However, this is not the case in reverse. Less than 5% of patients with achalasia develop an epiphrenic esophageal diverticulum, with the exception of those with ‘vigorous’ achalasia, as more pulsion forces are involved (Thomas et al., 2001).
Diffuse Esophageal Spasm and Other Motility Disorders
The second most common motility disorder found in patients with epiphrenic esophageal diverticulum is diffuse esophageal spasm (Herbella and Patti, 2012). This is characterised by “simultaneous, uncoordinated, or rapidly propagated contractions that are of normal amplitude and accompanied by dysphagia”. Once again, differential diagnosis is critical because there is a long list of disorders that resemble it (Goel and Nookala, 2023, July 2).
In one small study using high-resolution impedance manometry, other motility disorders associated with esophageal diverticulum include, in descending order of occurrence: esophagogastric junction outflow obstruction, jackhammer esophagus, ineffective esophageal motility and absent contraction (Yuan et al., 2024). Another small study by Carlson et al. (2016), which also used high-resolution manometry, revealed “propagating peristalsis, often with hypercontractility” as the predominant motility pattern in their participants.
I would recommend reading this paper by Nehra et al. (2022), which has some insightful explanations of the different types of motility disorders. There are tables which detail how they appear on diagnostic tests, their differentiating features, and the recommended examinations and treatments.
It is also important to note that motility disorders can stem from different dysfunctions. For instance, it could arise from an autoimmune disease (e.g. Scleroderma), impaired inhibitory innervation (e.g. distal esophageal spasm), or excessive cholinergic stimulation (e.g. hypercontractile/jackhammer esophagus) (Nehra et al., 2022).
In sum, it is important to be sure that what you have is truly an esophageal diverticulum, as the treatment and management plan can be quite different for each diagnosis. And since a motility disorder is often the underlying cause of epiphrenic esophageal diverticulum, it is important to investigate this further in order to reduce or eliminate the chance of recurrence.
Pin to Your Rare Disease & Motility Disorder Boards:
Esophageal Diverticulum Treatments
According to Varghese et al. (2007), “optimal surgical treatment is debated, mortality being 9% in the largest reported surgical series of 33 patients”. That’s not much data to go on. For epiphrenic esophageal diverticulum, the ‘traditional’ methods of treatment include: “transthoracic resection, long esophagomyotomy, and an antireflux procedure” (Varghese et al., 2007).
I won’t deep-dive into each treatment type here because honestly, I’m probably as clueless as you are. I think I’ve done sufficient research to ask my surgeon the questions I need to ask however, and his answers convince me that he knows what he is doing. So I will share only the treatments that piqued my interest initially, and also what I would personally need.
Diverticulum Peroral Endoscopic Myotomy (D-POEM)
I had read that diverticulum peroral endoscopic myotomy (D-POEM) is becoming more popular as a surgical method for esophageal diverticulum. It is a minimally-invasive procedure with various adaptations, but generally involves steps to create tunnels, dissect and reseal certain parts of the esophagus and its related muscles (Wang et al., 2020).
I was interested in D-POEM, because studies have shown that it has a high technical and clinical success rate, and also a low recurrence rate. It is also commonly used to treat achalasia and other motility disorders (Pelton et al., 2024). However, it has mostly been used for Zenker’s diverticulum, as compared to other types of diverticula (Mavrogenis and Bazerbachi, 2023).
In any case, I asked my surgeon about it. I didn’t quite understand his explanation of why it wouldn’t make sense to use it. He did say that the surgical treatment that I’d need would be the same regardless of diverticulum type however, which is a Heller myotomy.
Heller Myotomy and Fundoplication
Heller myotomy is the standard procedure used to treat achalasia, where the lower esophageal sphincter is cut to relieve pressure, so that food and liquid can pass through. Acid reflux can occur after a Heller myotomy, so a partial fundoplication may be done in addition (UCLA Health, n.d.).
A fundoplication is an anti-reflux surgical procedure, where a “gastric fold is wrapped around the distal esophagus which enforces the lower esophageal sphincter and prevents gastroesophageal reflux”. It can be either full (Nissen) or partial (Toupet, Dor or Thal) (Abdrabou et al., 2022, April 1).
A Dor fundoplication takes the frontal approach, whilst a Toupet or Thal fundoplication from the back (Abdrabou et al., 2022, April 1). The most common is a Dor fundoplication, where part of the stomach is wrapped over the front of the esophagus and stitched in place. Nissen fundoplication is rarely advised for patients with achalasia, as it can lead to issues with peristalsis (Northwestern Medicine, n.d.).
My surgeon also said that he would probably need to perform the surgery at two entry points, with one incision from near the abdomen. Since my right chest wall has been tunnelled through before in order to repair my mitral valve, a thoracic surgeon will be needed on the surgical team to help ‘navigate’ through the web of adhesions.
According to Torres-Villalobos and Martin-del-Campo (2013), “myotomy can be safely performed using open abdominal and thoracic approaches, and for more than two decades, it has also been done using laparoscopy and thoracoscopy”. I’m assuming that was what the surgeon meant when he was explaining it to me.
Potential Surgical Complications
The rate of symptom relief for esophageal diverticulum is between 85% to 100%, using standard treatments such as “laparoscopic myotomy, diverticulectomy, and fundoplication”. Having said that, the complication rate for the procedure itself is high (Herbella and Patti, 2012).
Some complications that can occur post-surgery include: “air leaks, septicemia and/or sepsis, mediastinitis, mediastinal empyema with or without fistula, mediastinal abscess, postoperative wound infection, and postoperative hemorrhage” (Onwugbufor et al., 2013).
Leaks are one of the more common complications post surgery, at a rate of up to 23%. My own surgeon has told me that a leak was his biggest concern. The mortality rate for the procedure reaches up to 7% as well (Herbella and Patti, 2012).
Your surgeon will most likely use a combination of procedures in order to treat you, based on several factors. Your individual anatomy needs to be accounted for, as well as the size and position of the esophageal diverticulum, comorbidities and more. Each surgical method has its own risks and merits. For instance, a left thoracotomy provides good access to an epiphrenic diverticulum, but is also associated with a high morbidity rate (up to 21% of patients had a leak), and a mortality rate of up to 11% (Herbella and Patti, 2012).
Here is a summarised table of optimal surgical treatments used to treat epiphrenic esophageal diverticulum from 17 published series (Sato et al., 2023).
Conclusion – There is Still So Much More to Learn About Esophageal Diverticulum
I hope that this article has given you some insight into the rare disease, esophageal diverticulum. I talked about epiphrenic esophageal diverticulum a little more, as that has a direct impact on me.
Doing research has helped me to cope with the helplessness and numbness I am currently feeling. Whenever I discover a correlation between my symptoms and an explanation from a medical journal, I feel enlightened or triumphant. To say that “knowledge is power” is underrated. Knowledge is healing. And we don’t know enough as it stands.
If you liked this article, sign up for our mailing list so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
Pin to Your Rare Disease & Chronic Illness Boards:

- Abdollahimohammad, A., Masinaeinezhad, N., & Firouzkouhi, M. (2014). Epiphrenic esophageal diverticula. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, 19(8), 795–797. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235103/
- Abdrabou, A., Kusel, K., & Knipe, H. (2022, April 1). Fundoplication. Radiopaedia. https://doi.org/10.53347/rID-35706
- Alicuben, E. T., Luketich, J. D., & Levy, R. M. (2023). Epiphrenic Diverticulum. In Pryor, A. D. & Hawn, M. T. (Eds), Operative Techniques in Foregut Surgery (2nd ed.), 1. Wolters Kluwer Health. Retrieved from https://books.google.com.sg/books?id=xmGvEAAAQBAJ&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false
- Carlson, D. A., Gluskin, A. B., Mogni, B., Koo, J., Sood, R., Lin, Z., & Pandolfino, J. E. (2016). Esophageal diverticula are associated with propagating peristalsis: A study utilizing high-resolution manometry. Neurogastroenterology & Motility, 28(3), 392–398. https://doi.org/10.1111/nmo.12739
- Chaudhry, S. R., & Bordoni, B. (2023, July 24). Anatomy, Thorax, Esophagus. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK482513/
- Cleveland Clinic. (2021a, April 6). Achalasia: A Disorder of the Esophagus. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17534-achalasia
- Cleveland Clinic. (2021b, August 4). Esophagus. Cleveland Clinic. https://my.clevelandclinic.org/health/body/21728-esophagus
- Cleveland Clinic. (2022a, April 28). Peristalsis. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22892-peristalsis
- Cleveland Clinic. (2022b, August 29). Mediastinum. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24113-mediastinum
- Cleveland Clinic. (2023a, September 29). Esophageal Diverticulum. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16977-esophageal-diverticulum
- Cleveland Clinic. (2023b, October 5). Esophageal Manometry Test. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/4952-esophageal-manometry-test
- Constantin, A., Constantinoiu, S., Achim, F., Socea, B., Costea, D. O., & Predescu, D. (2023). Esophageal diverticula: From diagnosis to therapeutic management—narrative review. Journal of Thoracic Disease, 15(2), 759–779. https://doi.org/10.21037/jtd-22-861
- Goel, S., & Nookala, V. (2023, July 2). Diffuse Esophageal Spasm. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK541106/
- Gyawali, C. P., Carlson, D. A., Chen, J. W., Patel, A., Wong, R. J., & Yadlapati, R. H. (2020). ACG Clinical Guidelines: Clinical Use of Esophageal Physiologic Testing. Official Journal of the American College of Gastroenterology | ACG, 115(9), 1412. https://doi.org/10.14309/ajg.0000000000000734
- Hentschel, F. (2022). Chronic fibrosing esophagitis with diffuse esophageal intramural pseudo-diverticulosis. JGH Open, 6(5), 287–291. https://doi.org/10.1002/jgh3.12750
- Herbella, F. A. M., & Patti, M. G. (2012). Modern pathophysiology and treatment of esophageal diverticula. Langenbeck’s Archives of Surgery, 397(1), 29–35. https://doi.org/10.1007/s00423-011-0843-2
- Hjern, F., Mahmood, M. W., Abraham-Nordling, M., Wolk, A., & Håkansson, N. (2015). Cohort study of corticosteroid use and risk of hospital admission for diverticular disease. British Journal of Surgery, 102(1), 119–124. https://doi.org/10.1002/bjs.9686
- Mavrogenis, G., & Bazerbachi, F. (2023). Peroral endoscopic myotomy for Zenker’s diverticulum without tunneling. Endoscopy, 55, E946–E948. https://doi.org/10.1055/a-2127-7402
- MedlinePlus. (2024a, August 27). Barium Swallow. MedlinePlus. https://medlineplus.gov/lab-tests/barium-swallow/
- MedlinePlus. (2024b, August 27). Fluoroscopy. MedlinePlus. https://medlineplus.gov/lab-tests/fluoroscopy/
- MedlinePlus. (2023, February 27). Differential Diagnosis: Test. MedlinePlus. https://medlineplus.gov/lab-tests/differential-diagnosis/
- Nehra, D., Lord, R. V., DeMeester, T. R., Theisen, J., Peters, J. H., Crookes, P. F., & Bremner, C. G. (2002). Physiologic Basis for the Treatment of Epiphrenic Diverticulum. Annals of Surgery, 235(3), 346–354. https://journals.lww.com/annalsofsurgery/abstract/2002/03000/physiologic_basis_for_the_treatment_of_epiphrenic.6.aspx
- Nehra, A. K., Sheedy, S. P., Johnson, C. D., Flicek, K. T., Venkatesh, S. K., Heiken, J. P., Wells, M. L., Ehman, E. C., Barlow, J. M., Fletcher, J. G., Olson, M. C., Bharucha, A. E., Katzka, D. A., & Fidler, J. L. (2022). Imaging Review of Gastrointestinal Motility Disorders. RadioGraphics. https://doi.org/10.1148/rg.220052
- Northwestern Medicine. (n.d.). Heller Myotomy. Northwestern Medicine. Retrieved 22 January 2025, from https://www.nm.org/conditions-and-care-areas/treatments/heller-myotomy
- Onwugbufor, M. T., Obirieze, A. C., Ortega, G., Allen, D., Cornwell, E. E., & Fullum, T. M. (2013). Surgical management of esophageal diverticulum: A review of the Nationwide Inpatient Sample database. Journal of Surgical Research, 184(1), 120–125. https://doi.org/10.1016/j.jss.2013.05.036
- Patel, D. A., Lappas, B. M., & Vaezi, M. F. (2017). An Overview of Achalasia and Its Subtypes. Gastroenterology & Hepatology, 13(7), 411–421. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5572971/
- Pelton, M., Kahaleh, M., & Tyberg, A. (2024). Peroral Endoscopic Myotomy for the Management of Esophageal Diverticula: Tunneling Forward. Techniques and Innovations in Gastrointestinal Endoscopy, 26(1), 56–67. https://doi.org/10.1016/j.tige.2023.12.003
- Rezaee, A., Niknejad, M., & Weerakkody, Y. (2024, December 17). Epiphrenic diverticulum. Radiopaedia. https://doi.org/10.53347/rID-20707
- Sanivarapu, R. R., Vaqar, S., & Gibson, J. (2024, March 20). Aspiration Pneumonia. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK470459/
- Sato, H., Takeuchi, M., Hashimoto, S., Mizuno, K., Furukawa, K., Sato, A., Yokoyama, J., & Terai, S. (2019). Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World Journal of Gastroenterology, 25(12), 1457–1464. https://doi.org/10.3748/wjg.v25.i12.1457
- Sato, Y., Tanaka, Y., Ohno, S., Endo, M., Okumura, N., Takahashi, T., & Matsuhashi, N. (2023). Optimal surgical approaches for esophageal epiphrenic diverticulum: Literature review and our experience. Clinical Journal of Gastroenterology, 16(3), 317–324. https://doi.org/10.1007/s12328-023-01765-2
- Sudarshan, M., Fort, M. W., Barlow, J. M., Allen, M. S., Ravi, K., Nichols, F., Cassivi, S. D., Wigle, D. A., Shen, R. K., & Blackmon, S. H. (2021). Management of Epiphrenic Diverticula and Short-term Outcomes. Seminars in Thoracic and Cardiovascular Surgery, 33(1), 242–246. https://doi.org/10.1053/j.semtcvs.2020.08.017
- Sudarshan, M., & Murthy, S. (2021). Esophageal Motility Disorders and Diverticula: Physiologic Implication and Surgical Considerations. Foregut, 1(3), 263–267. https://doi.org/10.1177/26345161211045613
- Thomas, M. L., Anthony, A. A., Fosh, B. G., Finch, J. G., & Maddern, G. J. (2001). Oesophageal diverticula. BJS (British Journal of Surgery), 88(5), 629–642. https://doi.org/10.1046/j.1365-2168.2001.01733.x
- Torres-Villalobos, G., & Martin-del-Campo, L. A. (2013). Surgical Treatment for Achalasia of the Esophagus: Laparoscopic Heller Myotomy. Gastroenterology Research and Practice, 2013(1), 708327. https://doi.org/10.1155/2013/708327
- UCLA Health. (n.d.). Esophageal Health – Esophageal / Heller Myotomy. UCLA Health. Retrieved 22 January 2025, from https://www.uclahealth.org/medical-services/gastro/esophageal-health/tests-treatments/surgical/esophageal-heller-myotomy
- Varghese, T. K., Marshall, B., Chang, A. C., Pickens, A., Lau, C. L., & Orringer, M. B. (2007). Surgical Treatment of Epiphrenic Diverticula: A 30-Year Experience. The Annals of Thoracic Surgery, 84(6), 1801–1809. tps://doi.org/10.1016/j.athoracsur.2007.06.057″ target=”_blank”>https://doi.org/10.1016/j.athoracsur.2007.06.057
- Wang, S., Chai, N., & Linghu, E. (2020). Diverticulum Peroral Endoscopic Myotomy (D-POEM). In Linghu, E. (Ed.), Therapeutics of Digestive Endoscopic Tunnel Technique (pp. 121–124). Springer. https://doi.org/10.1007/978-981-15-1998-7_9
- Watanabe, Y., Taniyama, Y., Koseki, K., Ishida, H., Ozawa, Y., Okamoto, H., Sato, C., Unno, M., & Kamei, T. (2023). Distinguishing Killian–Jamieson diverticulum from Zenker’s diverticulum. Surgical Case Reports, 9(1), 21. https://doi.org/10.1186/s40792-023-01599-7
- Yadlapati, R. (2017). High Resolution Manometry Vs Conventional Line Tracing for Esophageal Motility Disorders. Gastroenterology & Hepatology, 13(3), 176–178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5439137/
- Yam, J., Baldwin, D. L., & Ahmad, S. A. (2023). Esophageal Diverticula. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK532858/
- Yuan, M.-C., Chou, C.-K., Chen, C.-C., Wang, H.-P., Wu, J.-F., & Tseng, P.-H. (2024). Characteristics of Esophageal Motility and Associated Symptom Profiles in Patients with Esophageal Diverticulum: A Study Based on High-Resolution Impedance Manometry. Digestive Diseases and Sciences, 69(2), 510–520. https://doi.org/10.1007/s10620-023-08196-6
- Zakaria, A., & Barawi, M. (2020). Endoscopic treatment of Killian-Jamieson diverticulum using submucosal tunneling diverticulotomy technique. VideoGIE, 5. https://doi.org/10.1016/j.vgie.2020.05.031